Central Sleep Apnea (CSA) is a condition characterized by interruptions in breathing during sleeping and resting hours. This sleep disorder can either be present from birth, which is known as Congenital Central Hypoventilation Syndrome (CCHS), or be acquired later in life. Central Sleep Apnea functions very differently than Obstructive Sleep Apnea. Central Sleep Apnea stems from the brain not sending the appropriate signals to breathe, whereas Obstructive Sleep Apnea is caused by physical obstruction to the airway. Central Sleep Apnea is much rarer than Obstructive Sleep Apnea and some patients experience symptoms during periods of rest as well as while asleep.
Click here for more information on CCHS and how the Avery Diaphragm Pacing System can help
WHAT IS CCHS?
Researchers have found that Congenital Central Hypoventilation Syndrome is a congenital condition caused by a mutation in the PHOX2B gene. This gene’s job is to encourage the growth of nerve cells and ensure that the nerves are assigned a specific function. In the autonomic nervous system, the nerves affected by this mutation include those responsible for regulating breathing.
According to the National Institutes of Health, this disorder is very rare, with only 1,000 patients identified worldwide. It is believed that some children who die from Sudden Infant Death Syndrome (SIDS) may have had undiagnosed CCHS. Children can either develop this from a parent, which has become more common as CCHS patients are more frequently living into adulthood, or have a mutated gene. The latter reason accounts for 90% of cases.
CHARACTERISTICS OF CCHS
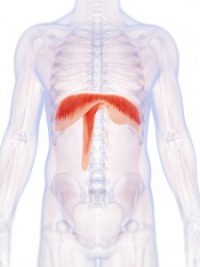
CCHS is characterized by breathing difficulties. Those who have the condition hypoventilate, or take very shallow breaths, which is worsened during sleep. Though most people view the condition as more severe at night, patients may also have breathing difficulties while awake. The result of these shallow breaths is that there is an increase in carbon dioxide in the blood and a decrease in critically needed oxygen. Normally, the autonomic nervous system regulates consistent involuntary breathing. In patients with CCHS, this involuntary function is not working. The brain “forgets” to tell the patient to breathe. For these patients, an Avery diaphragm pacemaker may be a lifesaving device.
CENTRAL SLEEP APNEA
With CSA, like CCHS, the brain lacks the ability to send signals to the diaphragm to breathe. Unlike CCHS, which is congenital, CSA develops during a person’s lifetime. It is typically caused by another health condition that impacts the brainstem. Because the brainstem is in control of sending signals to breathe, if there is any damage to this area, it is likely that breathing will be impaired.
Some of the ways patients develop CSA include:
- Stroke
- Brain tumor
CHARACTERISTICS OF CENTRAL SLEEP APNEA
While the patient is sleeping, his or her breathing stops cycling normally. The periods where the brain does not signal the body to breathe, called apneas, last for one to two minutes. After the periods of not breathing, the body then tries to overcompensate for the lack of oxygen by breathing faster for a period of time, known as a hyper-apnea. Depending on how long the apneas are, the damage CSA can cause may vary from person to person. When breathing is stopped for extended periods of time, brain damage may occur. Other risks caused by lack of oxygen to the brain include seizures, strokes or heart attacks.
CENTRAL SLEEP APNEA DURING THE DAY
CSA patients have an excess of carbon dioxide in the blood, presenting lingering side effects like difficulty breathing throughout the day. A malfunctioning brainstem is the root of the cause, in addition to the lower carbon dioxide levels. Though difficulty breathing during the day is possible, the most severe symptoms of Central Sleep Apnea happen during the night, as the autonomic nervous system operates differently during wakefulness than during sleep.
Patients with Central Sleep Apnea may experience daytime sleepiness and headaches as a result of their interrupted sleep cycles. They may also have difficulty concentrating and feel weak throughout the day. Being overly tired during the day can be how patients discover they are periodically not breathing during the night.
TREATMENT FOR CCHS/CENTRAL SLEEP APNEA
Because Central Sleep Apnea is often the result of another medical condition, the primary condition is typically treated first, in the hope that it will correct the breathing difficulties. When this is not possible, an Avery Breathing pacemaker may be an alternative to other forms of ventilation.
The Avery Biomedical Diaphragm Pacing System is a helpful option for patients with Central Sleep Apnea. The diaphragm pacing system is implanted surgically and stimulates the phrenic nerve which signals the diaphragm to contract at a normal rate. Because patients with Central Sleep Apnea never know when the apneas will occur, the pacemaker is consistently helpful, removing the risk of a lack of oxygen.
THE AVERY DIAPHRAGM PACING SYSTEM SYSTEM
The Avery Diaphragm Pacing System System is the only diaphragm-pacing device with full pre-market approval from the USFDA and CE marking privileges under the European Active Implantable Medical Device Directive for adult and pediatric use. In addition, its system of using small implanted radiofrequency receivers rather than electrode wires that pass directly through the skin may decrease a patient’s risk of infection and ongoing wound care management issues.
Avery has been commercially distributing diaphragm pacing systems since the early 1970s. Since then, more than 2,000 patients have been implanted in over 40 countries establishing an unsurpassed record of safety and reliability.