(Note: if you are familiar with the different types of sleep apnea and would like to jump straight to information on OSA masks leading to CSA, you can click here)
Sleep apnea is a sleep disorder characterized by pauses in breathing during sleep. There are multiple types of sleep apnea that can occur, and are similar in that they affect breathing. These are obstructive sleep apnea and central sleep apnea. While they are treated differently, and affect the body in very different ways, there is now evidence to suggest that some therapies for obstructive sleep apnea that can contribute to central sleep apnea.
CSA vs. OSA
It is important to understand the distinction between the two main types of sleep apnea when looking at the relationship between the two.
- Obstructive Sleep Apnea (OSA) is the sleep apnea that is more commonly known by most people. This form of sleep apnea is more common, and occurs when there is something partially or completely blocking (obstructing) the airway during sleep. This is often accompanied by snoring, which is tested for in most sleep studies in order to differentiate from other apneas.
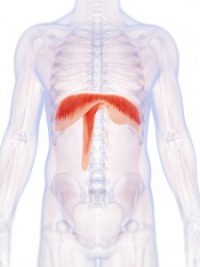
- Central Sleep Apnea Syndrome (CSAS or CSA) is characterized by pauses in breathing during sleep as a result of the brain not correctly using the neurological pathways to the diaphragm. Central sleep apnea events are typically silent, as a result of neurological issues as opposed to obstructive issues.
- There is also a form of sleep apnea called Complex Sleep Apnea Syndrome, which is a combination of OSA and CSA.
Symptoms of the types of sleep apnea are very similar, which is why it is important that diagnosis is performed by a doctor. The treatment methods also may differ significantly. Commonly, a CPAP mask is utilized for individuals with obstructive sleep apnea. However, there is evidence that CPAP masks may be linked to CSA in some individuals. This does not mean that a mask should not be used and that an individual shouldn’t follow the guidance of their physician. It does mean that if you or a loved one has OSA, they should be on the lookout for warning signs of CSA as well, know their options, and be ready to talk to their doctor about it should the need occur.
CPAP Masks Leading to CSA

The method often used to treat obstructive sleep apnea is a Continuous Positive Airway Pressure (CPAP) therapy. This typically consists of a mask that covers your nose and mouth (or in some cases, nose only), a tube that connects to a motor, and the motor to blow air into the tube. There is a condition known as CPAP emergent central sleep apnea, which develops while using CPAP therapy (masks).
CPAP emergent central sleep apnea, which is officially classified as “treatment emergent CSA,” is included in the International Classification of Sleep Disorders1.
CPAP emergent CSA often resolves over time, though it can persist (known as CPAP persistent CSA). In these cases, though a mask can help control the obstructive sleep apnea, the condition may worsen due to the onset of central sleep apnea. It was also found that patients who developed CPAP emergent CSA were more likely to stop CPAP therapy than those who did not.
In some studies, hypoventilation (when an individual’s breathing is too shallow or two slow to meet the needs of the body) is shown to manifest itself under positive airway pressure treatment. One such study states that “…disturbances of respiratory drive or the translation of central impulses may result in hypoventilation” and that “[central breathing disturbances during sleep] present as central sleep apnoeas…and can emerge under positive airway pressure treatment” (Definition, Discrimination, Diagnosis and Treatment of Central Breathing Disturbances During Sleep, also appearing in the European Respiratory Journal). Due to the potential link between obstructive sleep apnea treatments and central sleep apnea, it is important for those with OSA that may develop into CSA to know and understand all available treatment options.
Treatment for CSA
Any treatment for central sleep apnea must be provided under the care of your physician. CPAP machines, as noted, are a common therapy for sleep apnea. For many CSA patients, diaphragm pacing may be another option. Because CSA is not caused by an obstruction, but rather an issue with neurological pathways, a device may be used to create a more natural breathing pattern without the use of forced air from CPAP.
Rather than using positive pressure to force air into the lungs, the Avery Diaphragm Pacemaker stimulates the phrenic nerve, resulting in a more natural breathing pattern. As an FDA-approved device, the Avery Pacer may be utilized 24 hours per day, and is approved for use in both pediatric and adult patients.

The Avery Diaphragm Pacemaker has been featured in several studies and has been drastically improving lives for over three decades. It is the only diaphragm-pacing device with full pre-market approval from the USFDA and CE marking privileges under the European Active Implantable Medical Device Directive for adult and pediatric use.
Taking the Next Step
For more information on the Avery Diaphragm Pacemaker, please call us at 631-864-1600, or click the “request info” button below and fill out the contact form. We would be happy to get you more information about how the diaphragm pacing system may help, and connect you with a physician familiar with the device in your area if needed. If you’re looking for a physician, you can find a list of physicians and medical centers in the United States here, or find a list of international representatives here.
[fusion_button link=”/contact/” target=”_self” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” class=”request-info” color=”default” stretch=”default” icon_position=”left” icon_divider=”no” animation_direction=”left” animation_speed=”0.3″]Request Information About the Avery Diaphragm Pacing System[/fusion_button]
1 (American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar])